Please feel free to use our e-mail back service.
What is peri-implantitis?
Peri-implantitis is an inflammatory, irreversible process within the tissue surrounding an existing osseointegrated implant, leading to loss of supporting bone and therefore in due course to a loss of the implant. In comparison, peri-implant mucositis, an early stage of peri-implantitis, is a reversible inflammatory change to the peri-implant soft tissue without loss of bone.
The prevalence of peri-implant mucositis is stated at more than 50 percent, and peri-implantitis at 12 to 40 percent. Dentists consider the causes for peri-implantitis and the resulting loss of the implant to be functional overloading, general disease such as diabetes and osteoporosis, radiation and medication influences, smoking, poor oral hygiene, an untreated periodontally diseased jaw, lacking recall, as well as the design of the implant.
What is the relevance of peri-implantitis?
“Peri-implantitis … has a prevalence on the order of 10% of implants and 20% of patients 5 to 10 years after implant placement….”1
“Peri-implant diseases present in two forms – periimplant mucositis and peri-implantitis […] Outcomes from reports 4,5 assessing the prevalence of peri-implant diseases revealed that peri-implant mucositis was present in 48% of implants followed from 9 to 14 years affected with this problem. Since peri-implant mucositis is reversible with early intervention and removal of etiology, it is quite possible that its prevalence could be underreported.”2
1 Lisa J. A. Heitz-Mayfield, BDS, MDSc, Odont Dr /Andrea Mombelli, Prof Dr Med Dent (2014: The Therapy of Peri-implantitis: A Systematic Review in The International Journal of Oral & Maxillofacial Implants, S. 326 ff
2 AAP (2013): Peri-Implant Mucositis and Peri-Implantitis: A Current Understanding of Their Diagnoses and Clinical Implications; URL: http://www.joponline.org/doi/pdf/10.1902/jop.2013.134001, Status: 13.10.2014
What are the risk factors and the signs?
Risk Factors:
- Tobacco use
- High bite pressure
- Poorly controlled systemic conditions (e.g., diabetes mellitus, osteoporosis, post-irradiated jaws)
- History of periodontitis and noncompliance to treatment
- Poor oral hygiene
- Parafunctional habits (e.g., bruxism)
- Iatrogenic factors (e.g., lack of primary stability and premature loading during the healing period)
Signs:
- Progressive increase in probing depth
- Suppurations and exudation from peri-implant space
- Bleeding on probing
- Clinical appearance of inflamed tissue (bleeding, swelling, color change, suppuration, and plaque/calculus accumulation)
- Progressive loss of supporting bone on follow-up radiographs
Andrea Hsu, DMD, FRCD(C); Jung-Wan Martin Kim, DMD, FRCD(C) (2014): How to Manage a Patient with Peri-implantitis; URL: http://www.jcda.ca/article/e24, Status: 13.10.2014
Critical classes for peri-implantitis
Successful treatment is with the established therapies limited up to maximum class „C“ cases. With the innovative Er:YAG Morita therapy cases up to „D“ are covered.
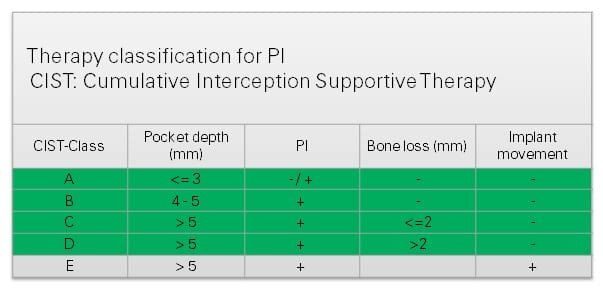
Francisco T. Carlos : Treatment Strategies for Peri-implant Diseases; URL: http://pbhsinform.com/Client/viewhtml.aspx?index=31364417-0220-42a5-ae6e-5ff9ff6a6652 , Status: 12.12.2014
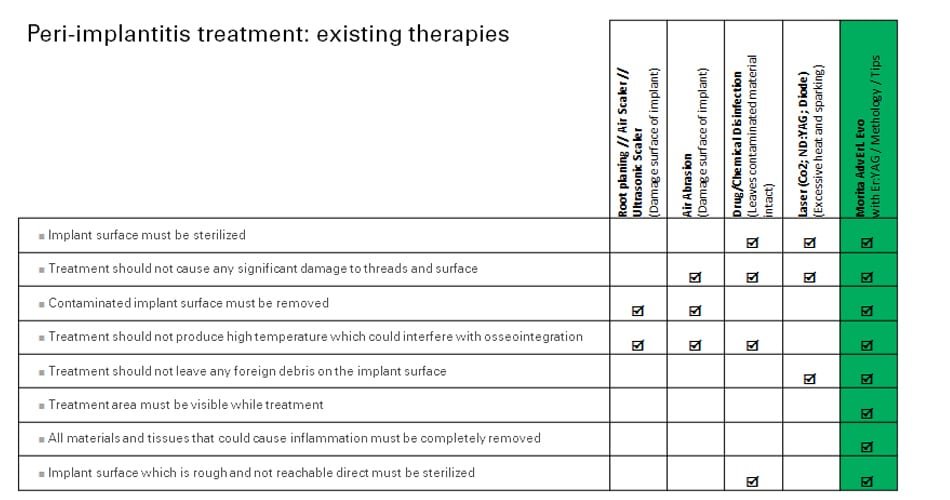
Preconditions for a successful treatment
- Implant surface must be sterilized
- Implant surface which is rough and not reachable direct must be sterilized
- Treatment should not cause any significant damage to threads and surface
- Contaminated implant surface must be removed
- Treatment should not produce high temperature which could interfere with osseointegration
- Treatment should not leave any foreign debris on the implant surface
- Treatment area must be visible while treatment
- All materials and tissues that could cause inflammation must be completely removed
Existing therapies
Methods for decontaminating implants and their drawbacks:
- Root planing (Damage surface of implant)
- Air scaler (Damage surface of implant)
- Ultrasonic scaler (Damage surface of implant)
- Air abrasion (Damage surface of implant)
- Chemical desinfection (Leaves contaminated material intact)
- Non Er:YAG lasers (Excessive heat and sparking)
Er:YAG laser AdvErL EVO for a successful treatment
The Er:YAG laser is used for treating the surface of the implant.
Causes of Peri-implantitis:
- Most implants have rough surfaces to increase surface area for enhanced osseointegration
- Increased surface area makes it difficult to reach and kill bacteria if the implant becomes contaminated




