Please feel free to use our e-mail back service.
From the beginning, endodontics has relied on imaging processes. As a rule, dental film images are used throughout the entire endodontic course of treatment and for assessing the outcome. However, X-rays are not infallible. Already 50 years ago, Bender and Seltzer (1), in their classic study, emphasized the fact that periapical lesions, which are limited to cancellous bone, cannot be recognized definitely. Numerous studies have been published, which demonstrate the limitations of conventional X-ray technology (1,2,3,4). Estrela et al. (5) compared the diagnostic precision of dental film and panoramic tomography to CBCT with regard to recognizing apical periodontal inflammation. They determined sensitivity of 0.55 and 0.28 for the dental film and panoramic tomography. Contrary to the diagnostic uncertainty of conventional X-rays mentioned above, it was possible to accurately determine the presence and size of the lesion in all cases with the help of CBCT (sensitivity for CBCT: 1.0). This allows the conclusion that CBCT diagnostics can be used as the new „gold standard“ for diagnosing the presence or absence of apical periodontal inflammation (5). These results were confirmed by many other studies (6,7). With the introduction of CBCT to dentistry in 1998, it also was possible to decisively improve diagnostics in endodontics because CBCT provided significantly more accurate images with reduced radiation dosage as compared to computer tomography (3).
Case 1:
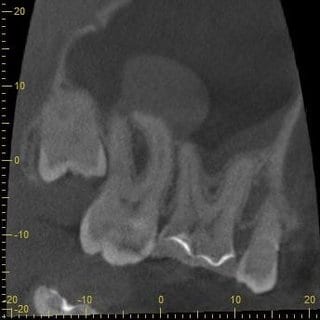
In this clinical case, a 48-year-old male patient was referred by his ENT physician for clarification of a dentogenic cause. The clinical and X-ray exams (Fig. 1 and 2) initially revealed no dentogenic cause for the problems on the right side of the face.
In further consultation with the ENT physician, who had actually requested a CT scan of the paranasal sinus, it was possible to convince him of performing a CBCT of this region, particularly because of the lower radiation dosage and higher resolution. The CBCT scan showed a clear-cut swelling of the maxillary sinus mucosa in the region of tooth 17 (Fig. 3 and 4). Maillet et al. (8) found that far more than 50% of cases with sinusitis maxillaris have a dentogenic cause, and in most cases the palatal root of the first molar, followed by the mesiobuccal root of the second molar, is responsible for this (8).
After consultation with the ENT physician, tooth 17 was treated endodontically. The complaints of the patient subsided after the treatment.
Fig. 5: Tooth 17 after endodontic treatment
A recall CBCT was performed two years after completion of the endodontic treatment after consultation with the ENT physician because no information about the state of the maxillary sinus, either before or after the treatment, was obtained from the dental film. Thereupon, as compared to the first scan, healing of the maxillary sinus mucosa can be seen on both section planes of the CBCT (Fig. 6 and 7).
Case 2:
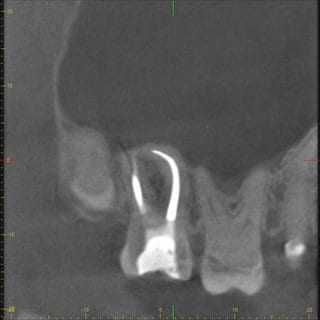
In the following clinical case, the 50-year-old male patient was referred to us for further treatment by his general dentist because the patient complained about persistent pain after a root canal treatment. The dental film (Fig.8) taken by the general dentist shows a sufficient root filling.
Fig. 8: Dental film of the dentist
Clinically the tooth showed a positive reaction to percussion, and the patient stated that pressure caused pain. The CBCT image taken by us revealed a non-prepared canal on the lingual side (Fig. 9 and 10). An endodontic treatment may fail because additional roots or canals are not detected and treated (9). In addition to the lingual canals and roots in the region of the anterior teeth and premolars of the lower jaw, the second mesiobuccal root canal of the upper molars frequently is the cause for additional treatment.
In the course of the final revision, both canals were prepared and filled with thermoplastic material. The patient already was without pain after the first session, which involved revision of the buccal canal and preparation the lingual canal.
List of references
(1) Bender IB, Seltzer S. Roentgenographic and direct observation of experimental lesions in bone. J Am Dent Assoc 1961;62:152-160.
(2) Bender IB. Factors influencing the radiographic appearance of bony lesions. J Endod 1997;23:5-14.
(3) Mozzo P, Procacci C, Tacconi A. A new volumetric CT machine for dental imaging based on the cone-beam technique: preliminary results. Eur Radiol 1998;8:1558-1564.
(4) Patel S, Mannocci F, Shemesh H, Wu MK, Wesselink PR, Lambrechts P. Radiographs and CBCT – time for a reassessment? Int Endod J 2011;44:887-888.
(5) Estrela C, Bueno MR, Leles CR, Azevedo BC, Azevedo JR. Accuracy of cone beam computed tomography and panoramic radiography for the detection of apical periodontitis. J Endod 2008;34:273-279.
(6) Patel S, Dawood A, Mannocci F, Wilson R, Pitt Ford T. Detection of periapical bone defects in human jaws using cone beam computed tomography and intraoral radiography. Int Endod J 2009;42:507-515.
(7) Stavropoulos A, Wenzel A. Accuracy of cone beam dental CT, intraoral digital and conventional film radiography for the detection of periapical lesions: an ex vivo study in pig jaws. Clin Oral Investig 2007;11:101-106.
(8) Maillet M, Bowles WR, McClanahan SL, John MT, Ahmad M. Cone-beam computed tomography evaluation of maxillary sinusitis. J Endod 2011;37:753-757
(9) Patel S, Durack C. Cone beam computed tomography in endodontics. Braz Dent J 2012;23:179-191